Arthritis is a common condition that affects millions of people worldwide, causing inflammation, stiffness, and pain in the joints. This debilitating condition can significantly impact your daily activities, mobility, and overall quality of life. While there is no cure for arthritis, there are various treatments and lifestyle adjustments that can help manage the symptoms and improve your ability to live well with arthritis. One of the most widely used methods of managing arthritis pain is through medication, specifically pills that reduce inflammation, alleviate pain, and help maintain joint function.
Understanding Arthritis
Arthritis is an umbrella term for more than 100 different types of inflammatory joint diseases. The most common forms of arthritis include:
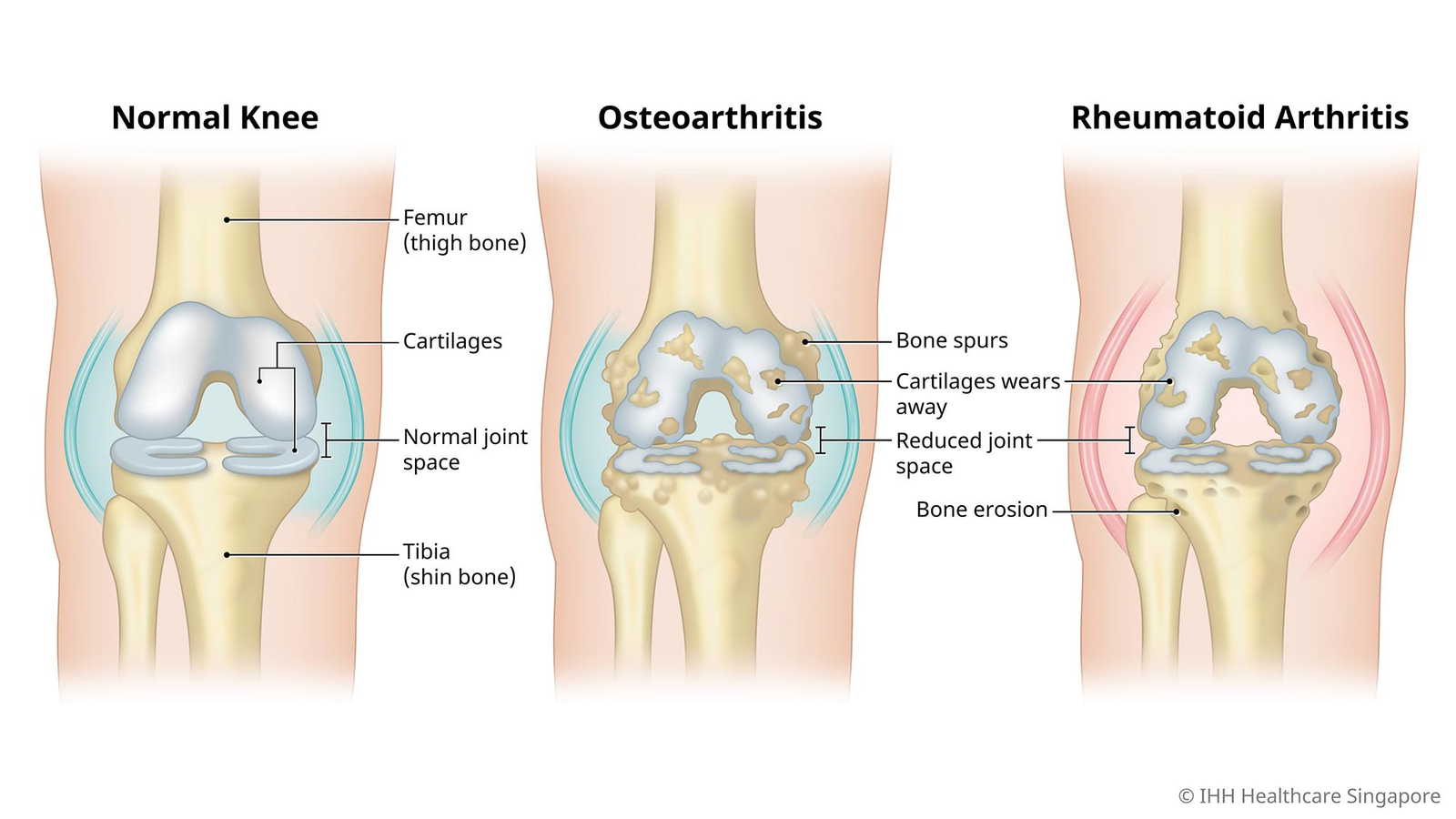
- Osteoarthritis (OA): A degenerative joint disease that occurs when the protective cartilage that cushions the ends of the bones breaks down, leading to pain, swelling, and stiffness.
- Rheumatoid Arthritis (RA): An autoimmune disorder where the immune system mistakenly attacks the lining of the joints, causing inflammation, pain, and potential joint damage.
- Psoriatic Arthritis (PsA): A form of arthritis associated with the skin condition psoriasis, which leads to joint pain, swelling, and skin rashes.
- Ankylosing Spondylitis (AS): A type of arthritis that primarily affects the spine, causing inflammation and pain in the back and hips.
Each type of arthritis has its unique symptoms and treatment approaches, but the goal of treatment is always to manage pain, reduce inflammation, and preserve joint function.
Treatment with Pills: A Key Component in Managing Arthritis
While lifestyle changes such as exercise, weight management, and joint protection techniques are essential in managing arthritis, medications play a crucial role in providing relief. Pills are often the first line of defense against arthritis pain, and a wide range of medications are available to address the different aspects of arthritis.
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
One of the most commonly prescribed medications for arthritis pain is NSAIDs. These drugs work by reducing inflammation, pain, and swelling. Over-the-counter (OTC) options, such as ibuprofen (Advil, Motrin) and naproxen (Aleve), are often used for mild to moderate pain. For more severe cases, a doctor may prescribe stronger NSAIDs, such as diclofenac (Voltaren) or indomethacin (Indocin).
How NSAIDs work: NSAIDs inhibit the production of cyclooxygenase (COX) enzymes, which are responsible for producing prostaglandins. Prostaglandins are chemicals that promote inflammation, pain, and fever. By blocking COX enzymes, NSAIDs help to reduce the pain and swelling associated with arthritis.
When to use NSAIDs:
- For short-term relief of flare-ups and joint pain
- To reduce swelling and inflammation during active stages of arthritis
- As part of a comprehensive arthritis management plan, alongside other treatments
Considerations: While NSAIDs are effective in managing arthritis pain, they can have side effects, especially with long-term use. These may include stomach irritation, ulcers, kidney problems, and increased risk of heart disease. It’s important to use NSAIDs as directed by a healthcare provider and avoid overuse.
2. Acetaminophen (Tylenol)
Acetaminophen is another common medication used for arthritis pain relief. Unlike NSAIDs, acetaminophen doesn’t reduce inflammation but works by blocking pain signals in the brain.
How acetaminophen works: Acetaminophen reduces the perception of pain in the brain without having any anti-inflammatory effects. It’s often used for mild to moderate pain and is considered a safer option for those who cannot tolerate NSAIDs.
When to use acetaminophen:
- For mild to moderate pain relief
- For individuals who have a history of stomach issues, ulcers, or heart disease
- As a supplement to other arthritis treatments
Considerations: Acetaminophen is generally well-tolerated, but it’s important to monitor your dosage, as excessive use can lead to liver damage. Avoid taking multiple medications that contain acetaminophen simultaneously.
3. Disease-Modifying Antirheumatic Drugs (DMARDs)
For individuals with rheumatoid arthritis or other inflammatory forms of arthritis, DMARDs are often prescribed to slow the progression of the disease and prevent joint damage. DMARDs don’t just manage symptoms; they target the underlying disease process itself.
There are two main types of DMARDs:
- Traditional DMARDs: These include methotrexate (Rheumatrex), sulfasalazine (Azulfidine), and hydroxychloroquine (Plaquenil). They work by suppressing the immune system to reduce inflammation and prevent joint damage.
- Biologic DMARDs: These newer medications, such as adalimumab (Humira) and etanercept (Enbrel), are designed to target specific components of the immune system that are responsible for inflammation in arthritis.
How DMARDs work: Traditional DMARDs work by suppressing the immune system, which is overactive in autoimmune forms of arthritis. Biologic DMARDs are more targeted and work by inhibiting the production of specific molecules that cause inflammation.
When to use DMARDs:
- For moderate to severe rheumatoid arthritis or other autoimmune types of arthritis
- When NSAIDs or acetaminophen are no longer sufficient for pain relief
- As part of a long-term treatment plan to reduce joint damage and improve quality of life
Considerations: DMARDs, especially biologics, can have serious side effects, including increased susceptibility to infections and liver damage. Regular monitoring by a healthcare provider is essential while taking these medications.
4. Corticosteroids
Corticosteroids like prednisone are potent anti-inflammatory medications that can quickly reduce pain and swelling in joints. They are often used for short-term flare-ups or to manage inflammation in conditions like rheumatoid arthritis or lupus.
How corticosteroids work: Corticosteroids mimic the effects of cortisol, a hormone produced by the adrenal glands. They work by suppressing the immune system and reducing inflammation throughout the body.
When to use corticosteroids:
- For acute flare-ups of arthritis
- When other medications are not effective in controlling pain or inflammation
- To provide temporary relief during a transition to other treatments
Considerations: Corticosteroids are generally not recommended for long-term use due to their potential side effects, including weight gain, osteoporosis, diabetes, and high blood pressure. Doctors usually prescribe them in low doses for short durations to minimize these risks.
5. Biologic Agents for Psoriatic Arthritis
For individuals with psoriatic arthritis, biologic agents like ustekinumab (Stelara) or secukinumab (Cosentyx) can be highly effective in targeting specific immune system pathways involved in both the joint and skin symptoms of the disease.
How biologic agents work: These medications are designed to block specific proteins, such as tumor necrosis factor (TNF) or interleukins, that promote inflammation in the joints and skin.
When to use biologics:
- For moderate to severe psoriatic arthritis
- When traditional DMARDs are not effective or tolerated
- To manage both skin and joint symptoms of psoriatic arthritis
Considerations: Biologic agents can suppress the immune system and increase the risk of infections, including serious ones. Regular medical check-ups are necessary while on biologics to monitor for side effects.
6. Pain Relief Medications and Opioids
For individuals with severe arthritis pain that doesn’t respond to NSAIDs or other medications, opioid pain relievers like hydrocodone or oxycodone may be prescribed. However, these are typically considered a last resort due to the risk of addiction and other side effects.
How opioids work: Opioids block pain signals in the brain and spinal cord, providing significant relief from severe pain. However, they do not address inflammation, and their long-term use can lead to dependence and other complications.
When to use opioids:
- For severe, unrelenting arthritis pain that hasn’t responded to other treatments
- For short-term use during acute flare-ups under the close supervision of a healthcare provider
Considerations: Opioids are generally not recommended for long-term use due to the risk of addiction, overdose, and other serious side effects. They should only be used as part of a comprehensive pain management plan that includes other treatments.
Lifestyle Adjustments for Managing Arthritis Pain
In addition to medications, there are several lifestyle changes that can help manage arthritis and improve quality of life:
- Exercise: Regular low-impact exercise, such as swimming, walking, or cycling, helps maintain joint function, reduce stiffness, and alleviate pain. Focus on strengthening the muscles around the joints to provide better support.
- Weight management: Maintaining a healthy weight can reduce the strain on weight-bearing joints, such as the knees and hips, helping to reduce pain and prevent further joint damage.
- Heat and cold therapy: Applying heat or cold to affected joints can help reduce pain and inflammation. Heat can relax stiff muscles, while cold packs can numb the area and reduce swelling.
- Joint protection techniques: Using assistive devices, such as braces or splints, and making modifications to your environment (e.g., installing grab bars, using ergonomic tools) can help protect joints and prevent further damage.
Conclusion
Living with arthritis is a challenge, but with the right combination of medications, lifestyle changes, and support, it’s possible to manage pain, improve mobility, and maintain a high quality of life. Pills such as NSAIDs, acetaminophen, DMARDs, and corticosteroids can play an essential role in controlling symptoms and preventing joint damage. However, it’s important to work closely with your healthcare provider to determine the best treatment plan for your specific type of arthritis, and to make necessary adjustments as your condition changes over time.
By incorporating appropriate medication with healthy lifestyle choices and coping strategies, those living with arthritis can continue to enjoy life, reduce pain, and preserve joint function.